Abstract
Introduction: Myelodysplastic syndromes (MDS) are a group of heterogeneous hematologic disorders of defective myeloid lineage maturation and differentiation. The Revised International Prognostic Scoring System (IPSS-R) is the most widely used prognostic model, and it incorporates the number of cytopenias, percentage of blasts, and cytogenetic abnormalities. The prognostic significance of eosinophilia is controversial (Wimazal et al, Cancer 2010) and is not part of the IPSS-R. We hereby evaluated the significance of eosinophilia in a cohort of MDS patients in our institution.
Methods: The clinical data for all patients diagnosed with MDS at Mayo clinic from October 1993 to March 2016 were reviewed after appropriate IRB approval was obtained. Patients with chronic myelomonocytic leukemia and MDS-excess blasts in transformation (blasts 20-29%) were excluded. Eosinophilia was defined as an absolute eosinophil count of >1 x109/L. The bone marrow biopsies, labs, and cytogenetic analysis at time of initial diagnosis for all cases were performed or reviewed at our center. Survival estimates were calculated using Kaplan-Meier curves, and univariate and multivariate analyses were based on log-rank testing using JMP software version 10.
Results: A total of 1222 patients with a confirmed diagnosis of MDS were identified (69% males). Median age at time of diagnosis was 71 years (range 18-99) and the median time of follow-up was 1.3 years. At time of last follow-up, 472 patients (38.6%) were still alive with a median overall survival of 2.4 years.
Only 12 patients (1%) were found to have significant eosinophilia at diagnosis (EOS+), with a median age of 71.5 years (52-89), and 58% being males. Median white blood cell count (WBC) was 8.8 x109/L, hemoglobin 9.4 gm/dL, and platelets 192 x109/L. On comparison with the rest of the group only WBC was found to be higher in EOS+ patients (8.8 vs 3.4, p<0.0001). On review of cytogenetic analysis, 3 of the 12 patients (25%) with significant eosinophilia were found to have 5q - Syndrome as opposed to 67 patients in the whole cohort (5%) (p=0.04). Three additional patients (25%) were also found to have chromosome 5 abnormalities, but did not fit the criteria for diagnosis of 5q - Syndrome. EOS+ patients' risk stratification per IPSS-R were 57%, 29%, and 14% for very low, low, and high risk compared to 16%, 34%, 20%%, 17%, and 14% for very low, low, intermediate, high and very high, respectively.
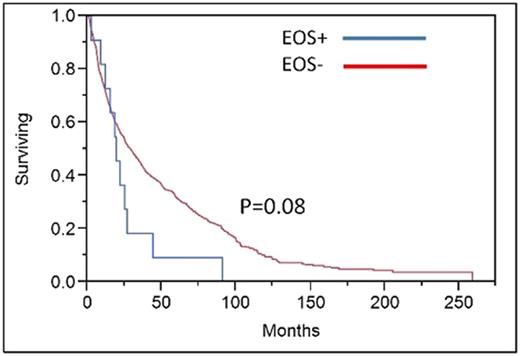
After median follow up of 1.3 years, EOS+ patients were more likely to be dead (92% vs 61%, p= 0.02). There was also a trend towards worse median overall survival (1.6 vs. 2.4 years, p=0.08). Only 1 of the 12 patients observed to have significant eosinophilia developed and died from progression to acute myeloid leukemia. On a multivariate analysis, age (P<0.0001), IPSS-R (P<0.0001) and EOS+ (hazard ratio =3.2, p=0.02) had statistically significant impact on OS.
Conclusion: Significant eosinophilia at time of initial diagnosis is an infrequent event in patients with MDS. EOS+ patients have a trend towards a worse overall survival. There was a higher frequency of chromosome 5 abnormalities in general, and 5q syndrome in particular, among patients with significant eosinophilia. The clinical significance of eosinophilia in this subset of patients is unknown but should be further explored as it might help further refine prognostication of these patients.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.